Remote patient monitoring (RPM) lets doctors and care teams check a patient’s health in real-time, without the patient being in a hospital. Devices like blood pressure monitors, heart rate sensors, glucose meters, or even tablets running care apps send data back to clinicians who can step in early if something’s wrong.
But for RPM to work, healthcare staff need secure, remote access to those devices, regardless if they’re in a patient’s home, a rural clinic, or a long-term care facility. That access must be fast, reliable, and fully protected from breaches.
In this article, we’ll explain how RPM works in real-world healthcare settings, where the security gaps often are, and how to improve remote patient monitoring with remote access technology without putting sensitive data at risk.
Remote Patient Monitoring Fundamentals
Remote patient monitoring isn’t new, but how it’s implemented today is changing the way healthcare systems operate at scale. RPM uses connected medical devices to collect and send health data from patients outside traditional clinical settings, usually from their homes, directly to healthcare providers in real-time or near-real time.
At its core, RPM is a system. Devices like Bluetooth-powered blood pressure cuffs, glucose monitors, or digital weight scales send readings to a central platform via a tablet, smartphone, or cellular hub. From there, that data is pushed to a remote care team that monitors for trends, flags anomalies, and contacts the patient if intervention by a health administration is needed.
This process relies on one thing: reliable and secure remote access. Whether we’re talking about an IT admin patching a hospital’s RPM hub or a nurse logging in to troubleshoot a patient’s tablet, the connection layer must work every time and never expose sensitive health data in the process.
RPM comes with a series of pros:
- Operationally, it frees up hospital beds, reduces in-person appointments, and improves workforce flexibility.
- For patients, it allows them to stay home longer, manage their care more independently, and receive faster intervention when something’s off.
- Continuous remote monitoring allows for more timely interventions before acute medical issues arise.
We use RealVNC Connect remote access software pretty much anywhere we can, from PCs to servers, to virtual desktops. It's so light, cost effective, and easy to use.
Ben Littleton
Systems and Network Manager, Sothern Ohio Medical Centre
With RealVNC, healthcare staff can automate admin-intensive tasks like diagnostic checks, mass device updates, and patch management. Plus, you can access and control devices remotely, including “headless” equipment.
Improve your healthcare service with secure remote access.
What to watch out for with a remote patient monitoring system
- Unsecured remote access to devices opens the door to patient data breaches, especially if IT relies on legacy tools that weren’t built for healthcare or compliance (like RDP without encryption or personal-use remote desktop tools).
- Device downtime, especially if a device loses connection or requires updates, as patients can go days without monitoring which puts them at risk.
- Scalability issues, due to situations such as RPM growing from 10 patients to 10,000. For this reason, you’ll need a top remote access solution to centralize management, auditing, and user access control.
The architecture of a RPM solution
RPM’s architecture comprises five fundamental components:
- Monitoring devices – these include wearables and sensors that track vital signs such as heart rate, low vs. high blood pressure, and glucose levels. Devices like smartwatches, blood pressure monitors, and glucose meters are common in this area.
- Data collection tools – these tools capture the data generated by monitoring devices. They can include mobile applications or embedded systems within the devices themselves.
- Transmission systems – once collected, patient data monitored remotely travels through secure transmission systems. These systems use encrypted channels that upkeep the safety of sensitive information as it moves from the patient to care team members.
- Analytical software – this component is of great importance for interpreting vast amounts of data, analyzing patterns and trends, and offering personalized insights. The human element is essential here, as only through professional health-related education one can truly interpret data in relation with the patient’s health status.
- Provider interfaces – the final component helps health providers access and interact with patient data efficiently. These interfaces, often integrated within existing healthcare management systems, enable providers to make informed decisions based on continuous data streams.
Key Benefits of Remote Patient Monitoring
Remote patient monitoring (RPM) offers a series of great advantages. This technology makes managing patient health more proactive, which is especially beneficial for chronic disease management.
Clinical benefits
In a Mayo Clinic study of nearly 5,800 patients enrolled in a remote patient monitoring (RPM) program, those who actually used the technology, by sending in at least one set of vitals, saw better health outcomes across the board.
Patients who engaged with the RPM system were less likely to be hospitalized, less likely to need intensive care, and had shorter hospital stays overall. They also had lower healthcare costs within the first 30 days and were less likely to die from any cause during that period.
But that’s not all. A comprehensive meta-analysis of 58 systematic reviews and numerous primary studies supports RPM’s effectiveness in chronic disease management. For heart failure patients, 17 systematic reviews confirmed that RPM reduces mortality, improves quality of life, and lowers healthcare costs
Financial advantages
RPM reduces healthcare costs because it minimizes hospital readmissions, leads to fewer emergency room visits, and strips away the unnecessary in-office consultations. Studies show that RPM can reduce hospital readmissions by 38% for chronic condition patients.
This cost-effectiveness translates into substantial savings for both patients and healthcare systems. For patients, this means fewer travel expenses and lower out-of-pocket costs, while healthcare systems benefit from reduced strain on resources.
Remote patient monitoring is now widely reimbursed by Medicare and most private insurers, which makes it more accessible (typically costing patients around $25 a month after deductibles are met).
Fewer in-person visits for chronic conditions free up clinic time for patients who truly need hands-on care that can’t be done remotely.
Patient satisfaction
A large-scale survey conducted by Mayo Clinic across multiple sites and regions found that remote patient monitoring (RPM) is not only clinically effective but also highly valued by patients. Out of over 3,000 respondents, 94% were satisfied with their RPM experience, and nearly 89% felt more comfortable managing their health from home.
Overall, remote patient monitoring helps patients catch health issues early, avoid unnecessary hospital visits, and stay in touch with care teams without leaving home. It reduces travel, supports medication adherence, and gives patients more control over managing chronic conditions. Many also report feeling safer and more connected, especially those living in rural areas or managing complex, ongoing treatments.
Access to specialist care
RPM bridges the gap for rural patients or those facing locomotor disabilities, who might otherwise face barriers to accessing specialist care. With remote monitoring, these patients can receive expert consultations and ongoing management without the need to travel long distances. Hence, RPM brings equitable treatment for underserved populations.
Chronic disease management
Remote patient monitoring solutions are particularly effective in managing chronic diseases. Through real-time health data, RPM allows for timely adjustments to treatment plans. Patients benefit from stable management of conditions like diabetes and heart disease, which translates to improved long-term outcomes. This is especially beneficial for those who suffer from acute and chronic conditions, such as the chronic obstructive pulmonary disease, as continuous data access allows healthcare providers to better engage with these patients.
Essential Remote Patient Monitoring Devices
Remote patient monitoring (RPM) comes in different types of monitoring devices, which we’ll explore below.
Blood pressure monitors
Blood pressure monitors with Bluetooth connectivity have become indispensable in RPM. These devices boast remarkable accuracy and offer reliable data for healthcare providers. Patients can use these monitors at home, as they transmit readings directly to medical professionals. The real-time data helps clinicians identify potential hypertension issues early.
Continuous glucose monitors
Continuous glucose monitors (CGMs) are essential for managing diabetes. These devices automatically transmit glucose readings every five or so minutes, which provides an up-to-date view of a patient’s blood sugar levels. This constant monitoring allows for precise adjustments to treatment plans and minimizes the risk of complications.
Pulse oximeters
Pulse oximeters are crucial for assessing blood oxygen levels and pulse rates. With a 94% sensitivity for detecting health deterioration, these devices alert healthcare providers to potential respiratory issues. Patients with chronic conditions such as COPD or asthma benefit significantly from regular monitoring. Secure remote access through RealVNC Connect allows clinicians to identify trends and intervene promptly, enhancing patient care.
Wearable health trackers
Wearable health trackers, such as smartwatches, offer a comprehensive view of vital signs, including heart rate, physical activity, and sleep patterns. These devices encourage patient engagement as they provide real-time feedback on their health status.
Security and Privacy Essentials for Remote Patient Monitoring
Remote patient monitoring (RPM) can only work at scale if the data stays secure. You’re dealing with deeply personal information, like heart rates, glucose levels, treatment history, and sometimes even video feeds from inside patients’ homes. If that data leaks, it’s a trust issue, a legal risk, and in some cases, a patient safety concern.
1. Encryption must come as standard
PM data should be encrypted both in transit (as it moves from the patient to the provider) and at rest (when it’s stored in cloud systems or local servers). Without this, intercepted data is readable. With it, it’s just scrambled noise to outsiders.
If a blood pressure reading is sent from a patient’s tablet to a hospital system, and that Wi-Fi is compromised, encryption makes sure no one can interpret the information without the correct decryption key.
2. Access controls protect the door
Passwords alone aren’t enough. Use multi-factor authentication (like an app-based code, preferably not an SMS code because those can be intercepted), restrict access by user role, and regularly remove former employees or unused accounts.
For example, a nurse might only need read-only access to a patient’s vitals, while an IT admin might need deeper access to maintain the system. Don’t give both the same privileges.
3. HIPAA compliance isn’t optional
In the U.S., HIPAA sets the stage for how to protect patient data, and RPM programs must align with it. That means regular audits, written security policies, breach protocols, and proof that staff have been trained in data handling.
If a device storing patient data is lost, HIPAA requires a documented response. That includes notifying affected patients and possibly regulators if data was exposed.
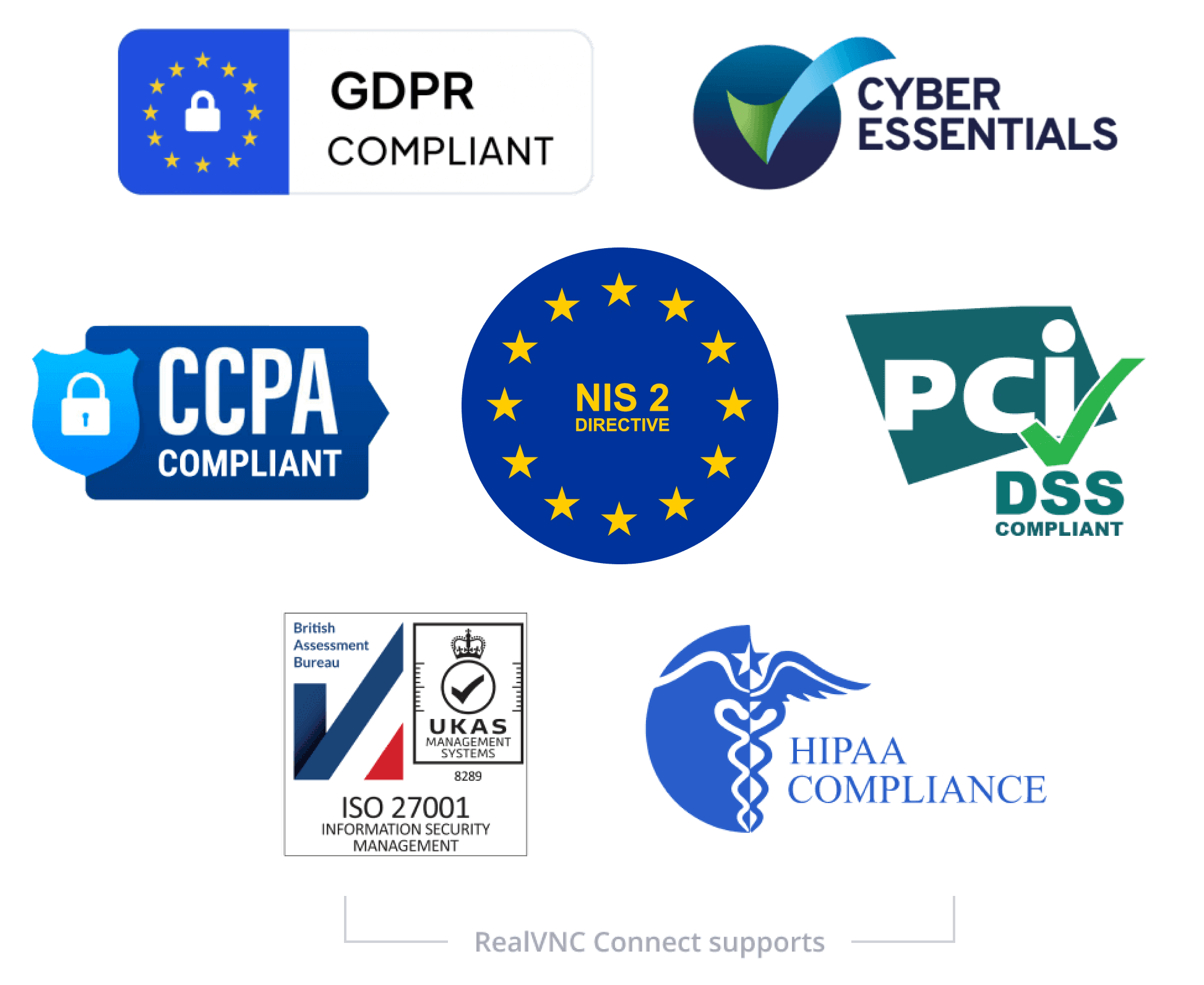
Did you know that RealVNC is compliant with HIPAA, GDPR, and more?
-
STANDARDS
AND COMPLIANCE -
DATA
PRIVACY -
SECURE
INFRASTRUCTURE -
24X7 SECURITY
OPERATIONS CENTER (SOC)
Standards and Compliance
RealVNC’s remote access solution is designed to meet and assist with a broad range of industry and government standards and regulations.
We are certified to ISO/IEC 27001:2013 and Cyber Essentials and comply with GDPR, and CCPA, ensuring adherence to stringent data protection and privacy guidelines. Additionally, RealVNC supports your compliance with HIPAA, PCI-DSS, and the new EU NIS2 directive. Download our NIS2 white paper to learn how RealVNC helps organizations align with the latest security requirements.
Data Privacy
RealVNC does not process, store, or have any access to any data accessed during a remote session.

Secure Infrastructure
The RealVNC Connect services run on RealVNC owned and managed servers and network equipment.
We do not use public Cloud services (such as AWS or Azure) for the RealVNC authentication and cloud connection brokering services. No third-party provider has access to the RealVNC infrastructure.
24x7 Security Operations Center (SOC)
We have a 24×7 Security Operations Center that monitors for cyber security events across our infrastructure and investigates and, where needed, mitigates them.
Global threat intelligence provides detailed information on attacker tools, techniques, and trends to facilitate effective triage.

4. The patient’s home is now part of your network
One overlooked risk in RPM is an unsecured home Wi-Fi. If a patient’s router is outdated, has a weak password, or has remote management enabled by default, it’s a wide-open backdoor. Providers should offer patients simple, non-technical guidance like:
- Change the default router password.
- Turn off remote access.
- Use WPA2 or WPA3 encryption.
5. Storage matters
Storing patient data in Excel files or personal drives is a disaster waiting to happen. All data should live in secure, encrypted environments (ideally cloud-based systems with permission tiers, logs, and built-in backup).
RealVNC Connect uses AES-GCM 128/256-bit encryption and Perfect Forward Secrecy, meaning even if someone were to capture encrypted traffic, they couldn’t ever decrypt it, not now, not later. That’s critical in healthcare, where data must remain protected for years.
Implementing Remote Patient Monitoring: A Simple Guide
Too often, remote patient monitoring (RPM) gets treated like a plug-and-play solution. In reality, successful adoption depends on how well your systems, staff, and workflows are aligned behind the scenes. Whether you’re a hospital, clinic, or outpatient care team, here’s how to set up an RPM program that actually works and scales.
1. Assess your organizational needs
Before buying any hardware, ask: Who are we helping, and why? RPM is most effective for patients with chronic conditions like hypertension, diabetes, heart failure, or COPD. These patients often account for the highest readmissions, which makes them ideal candidates for RPM support.
PS: You can use your EHR data to identify high-utilization patients or frequent readmissions in the last 6–12 months.
2. Choose the Right Devices
Match devices to your use case. For blood pressure use FDA-cleared monitors with Bluetooth or LTE transmission. For diabetes consider continuous glucose monitors with real-time syncing. Avoid overly complex tech, as patients won’t use it.
For example, a simple cellular-enabled scale helped one RPM program reduce heart failure readmissions by 40%, because patients used it daily without needing Wi-Fi.
3. Identify and enroll the right patients
Don’t throw RPM at everyone. Start with a small cohort who’ll benefit most. Good candidates are:
- Medically stable but need regular check-ins
- Comfortable with basic technology (or have a caregiver who is)
- Open to home-based monitoring
PS: RealVNC Connect can make onboarding easier by allowing IT teams to remotely walk patients through setup, device activation, or troubleshoot early issues.
4. Train your internal team
Your clinical and IT teams must know how to manage RPM, not just the tech, but what to do with the data.
- Clinicians should be trained on how to interpret real-time readings, recognize alerts, and escalate issues.
- IT should know how to manage remote devices securely using remote access software, without needing in-home access. To streamline this part, use RealVNC’s audit logging and access controls to monitor who’s accessing what, and keep both compliance and workflows tight.
5. Define clear monitoring protocols
Decide up front what data to collect, how often, and what triggers a nurse callback vs. a doctor escalation. For example:
- Blood pressure spikes above 180/110 = urgent callback
- Glucose drops below 70 mg/dL = automatic alert sent to care coordinator
Standardize this across your organization using digital care pathways or RPM software dashboards.
6. Set up secure, scalable tech
Security is a foundational part of RPM services, as it is the pillar behind safeguarding patient data, health facilities’ data, useful statistics, and more. When choosing a RPM system, security and scalability should be your number one decision factors. With RealVNC Connect:
- Every device is protected with end-to-end encryption and granular access controls
- You can run audits and monitor usage across your RPM fleet
- And you avoid complex network setups (no open ports, no inbound firewall rules needed)
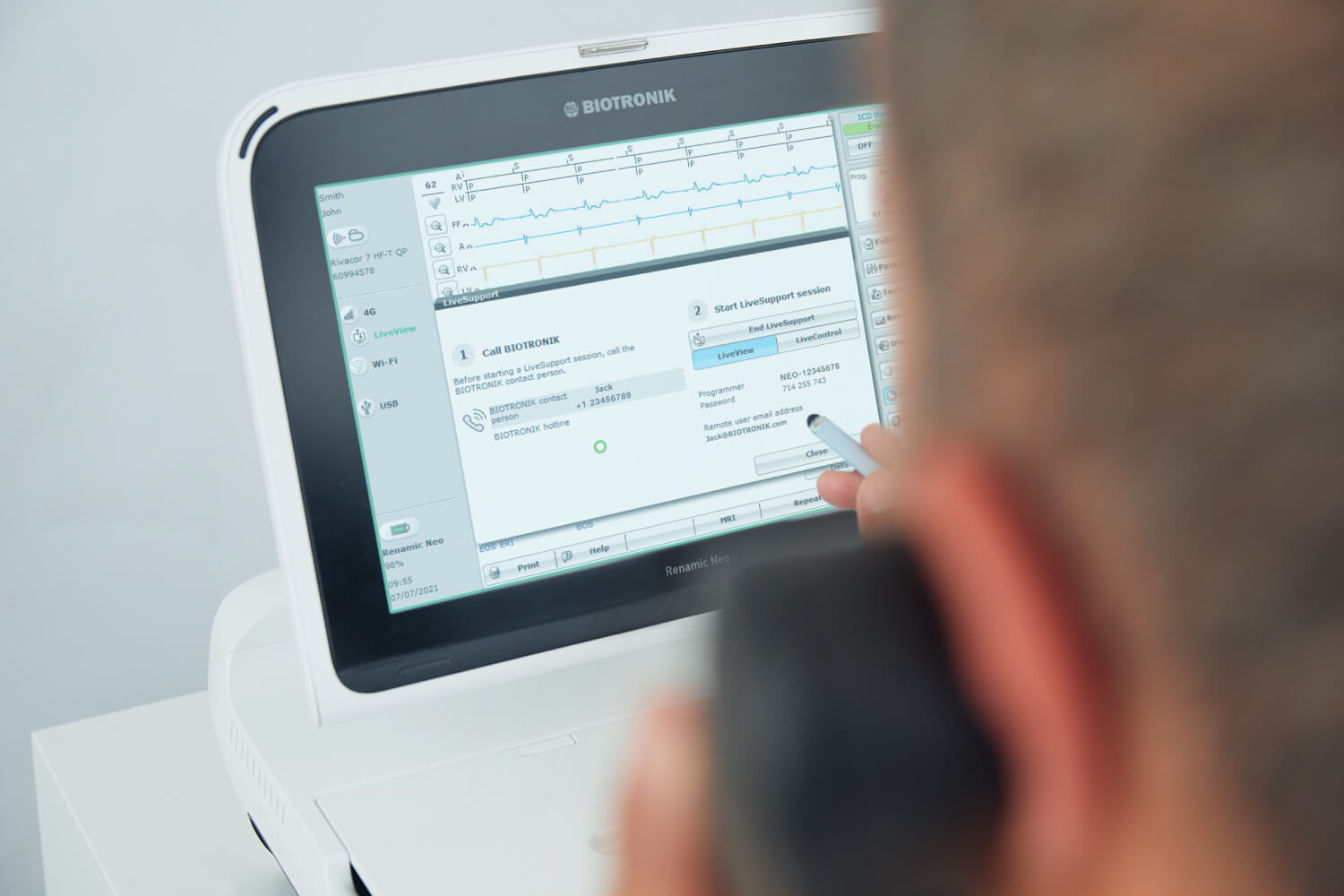
How BIOTRONIK Used RealVNC to Rethink Cardiac Device Support and Boost Patient Safety
BIOTRONIK, a global leader in cardiac implants, faced challenges offering real-time, on-site support for clinicians using its pacemaker programming devices. Limited to phone support and manual file transfers, engineers often had to travel long distances, even for a five-minute task, delaying care.
By integrating RealVNC Connect into its Renamic Neo device, BIOTRONIK launched LiveSupport, which brings secure, remote access in real-time.
Engineers can now see exactly what’s happening, take control when needed, and support implant procedures remotely. This reduced travel, improved service quality, and boosted patient safety.
7. Run a pilot before you scale
Choose 20–50 patients and track these metrics:
- Device usage rate
- Data submission consistency
- Clinical interventions triggered
- Patient satisfaction (via surveys)
- Number of tech support requests
Use what you learn to refine workflows and permissions within RealVNC Connect. Adjust training, alerts, and escalation protocols before scaling system-wide.
Here’s what to track as part of your RPM implementation:
- Patient adherence to monitoring protocols. Track how often patients submit their readings (e.g., weight, blood pressure, glucose) and whether they use the devices consistently. Non-adherence is one of the top reasons RPM programs underperform. Consider setting thresholds, like daily engagement rates or missed submissions, to trigger follow-ups. Tools like RealVNC Connect can help troubleshoot device issues remotely to reduce drop-offs caused by tech confusion.
- Reduction in hospital readmissions. Compare 30-day readmission rates before and after RPM adoption, especially for chronic conditions like heart failure or COPD. Flag unplanned ER visits or ICU escalations early to adjust care plans.
- Improvement in chronic disease management outcomes. Measure health markers relevant to each patient’s diagnosis, like HbA1c for diabetics or systolic blood pressure for hypertensive patients. Are these metrics trending in the right direction? Set clear baselines and use dashboards to show progress over time. RPM is most powerful when tied to measurable disease improvement..
RealVNC Connect: The Secure Foundation for Remote Patient Monitoring
If a remote patient monitoring (RPM) program fails, it’s usually because of one of three things: tech issues that go unresolved, patient data exposed through poor security, or workflows breaking across platforms. RealVNC Connect tackles all three.
Let’s start with access. RPM programs often rely on distributed devices, tablets, hubs, vitals-monitoring tools, placed in patients’ homes. When something goes wrong, support can’t wait for a site visit. RealVNC Connect allows your team to access those devices in real time, securely and without needing the patient to do anything complicated.
It’s built for healthcare-level security:
- End-to-end encryption (AES-GCM 128/256-bit with Perfect Forward Secrecy)
- Zero session storage – sessions aren’t recorded, ever
- No open inbound ports – far fewer attack surfaces
- HIPAA-ready with centralized audit logs and granular access control
And yes, it works across Windows, macOS, Linux, and Android-based RPM devices, without needing multiple remote tools.
FAQs of remote patient monitoring
What is remote patient monitoring?
Remote patient monitoring (RPM) refers to the use of connected devices, like blood pressure cuffs, pulse oximeters, or weight scales, to collect and transmit patient health data from their home to their care team. It shifts part of clinical monitoring outside the hospital or clinic, which allows for earlier interventions and continuous oversight without constant in-person visits.
How does remote patient monitoring work?
RPM combines medical-grade devices with software platforms that transmit health metrics in real time or at scheduled intervals. Data flows securely from the patient’s device (e.g., via cellular, Wi-Fi, or Bluetooth) to a cloud dashboard or EHR-integrated system. Clinicians receive alerts for out-of-range values, allowing them to act on trends before they escalate. Tech support tools, like RealVNC Connect, are often layered in to keep the system running without needing to send IT staff on-site.
What are the benefits of remote patient monitoring?
RPM helps reduce hospital readmissions, lowers care costs, and increases early detection of complications. For chronic condition management (e.g., heart failure or diabetes), RPM improves medication adherence, reduces ER visits, and supports personalized care.
What is an example of remote monitoring?
A practical example is a patient with heart failure using a Bluetooth-connected scale. The device sends daily weight data to their cardiologist. If a sudden gain indicates fluid retention, the care team is alerted, enabling early medication adjustment. A specific example of remote monitoring is using a continuous glucose monitor, which tracks blood sugar levels and transmits data every five minutes to healthcare providers for real-time management of diabetes.
Who pays for the RPM device?
Coverage varies. In the U.S., Medicare covers RPM for eligible conditions, typically under CPT codes 99453–99458. Most private insurers follow Medicare’s lead. Patients may pay a monthly co-pay (e.g., ~$25/month), but the device and software are often included in the provider’s program. Coverage outside the U.S. depends on national health systems and insurance models.
What are the key components of remote patient monitoring?
RPM systems include:
- Monitoring devices (e.g., BP monitors, ECG patches)
- Data gateways (smartphones/tablets or hubs)
- Secure transmission (cellular/Wi-Fi + encryption)
- Analytics platform for alerts and triage
- Clinician dashboards and EHR integration
- Support systems like RealVNC Connect for remote tech troubleshooting
How does RealVNC Connect support remote patient monitoring?
RealVNC Connect helps RPM programs function without interruption. When patients have tech issues with tablets or monitoring hubs, providers can use RealVNC to securely connect and fix problems in real-time, without relying on patients to troubleshoot, or sending field teams. It’s cross-platform, HIPAA-ready, and allows for faster intervention when system downtime could delay care.